As part of the Parkinson’s lecture series hosted by Charco, we had the pleasure of hearing from Nurse Nicola McQueen, a Specialist Parkinson’s nurse at Addenbrooke’s Hospital and a member of Charco’s Community Support Team. Nicola shared her expertise in preparing for hospital stays and making the most of Parkinson’s nurse support, sharing practical advice for those who may not have access to a specialist nurse in their area.

Nicola is a Parkinson’s specialist nurse based at Addenbrooke’s Hospital in Cambridge. She works alongside PD Consultants and other multidisciplinary teams (MDT) to ensure the best possible care is provided to people with Parkinson’s.
The Role of a Parkinson’s Nurse

Parkinson’s nurses play a crucial role in both the hospital and the broader community, ensuring comprehensive and timely support for people with Parkinson’s. Since 1996, Parkinson’s UK and The Excellence Network have supported the hiring of Parkinson’s nurses by proving through pump priming that specialist Parkinson’s nurses effectively pay for themselves. Parkinson’s nurses reduce hospital stays as well as incidences of falls and support people with Parkinson’s in maintaining independence and mobility – enabling savings to be made across health and social care services.
Medication Management:
- For those taking Parkinson’s medications, it’s crucial to get the right dose at the right time. Parkinson’s nurses provide guidance on managing Parkinson’s symptoms and medications, ensuring that patients receive the right advice for their condition.
Daily Responsibilities in Hospital:
- Every morning, Parkinson’s nurses review a list of patients with Parkinson’s who have been admitted to the hospital. They check each patient when they are admitted to make sure their medications are prescribed correctly and on time, following the ‘Get It On Time’ guidelines.
- The nurses also review any missed medications daily and weekly, providing education and support to address any issues.
Support and Education:
- Parkinson’s nurses regularly teach hospital staff about Parkinson’s medications, symptoms, and the importance of getting medications on time.
- Beyond hospital care, they advise medical and therapy teams on Parkinson’s treatment and train ‘Parkinson’s Champions’[link] on each hospital ward to create a network of knowledgeable supporters.
Emergency Support and Post-Discharge Coordination:
- They offer advice on medications outside regular hours and ensure there are emergency Parkinson’s medication cupboards stocked and available. They work with the on-call neurology team and ensure the pharmacy reviews Parkinson’s medications within 24 hours.
- They review cases in the emergency room to facilitate quick discharges, make referrals to specialist teams when needed, and communicate with community care teams upon a patient’s discharge from Hospital.
- When patients are discharged from the hospital, Parkinson’s nurses coordinate with community Parkinson’s nurse teams to ensure continuity of care and support.
Multidisciplinary Team Involvement:
- They are able to make referrals to other healthcare professionals as part of a multidisciplinary team (MDT).
- They also support the medical and therapy teams by offering expert advice on Parkinson’s care.
Family Support:
- Another key role of Parkinson’s nurses is to provide comprehensive support not only to people with Parkinson’s, but also to their families and carers, helping them navigate the challenges of the condition.
- Parkinson’s nurses are able to advise on medication and equipment, as well as other services such as mental health support, financial support that may be available, and symptom management through specialist teams and support or exercise groups in the area.
Tips for Hospital Admission
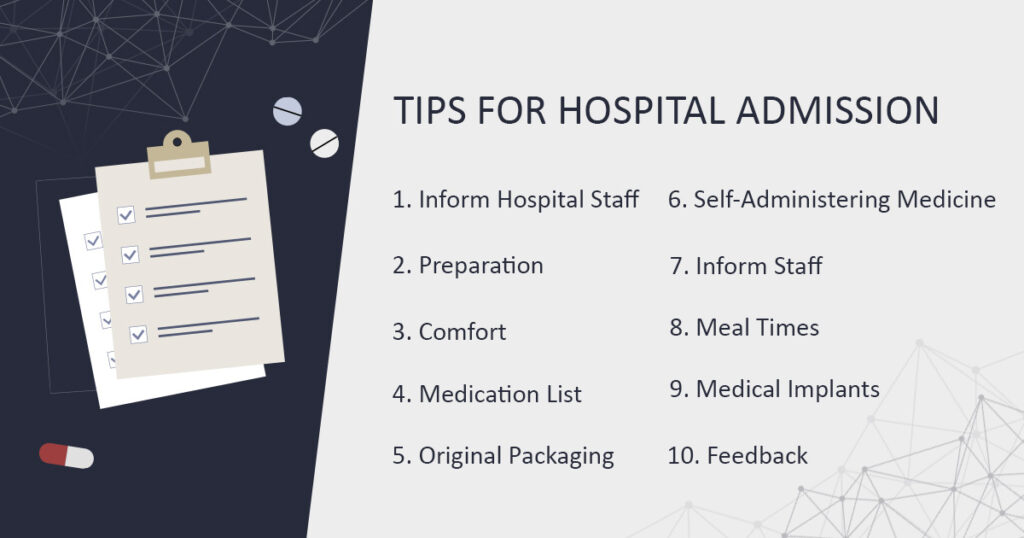
Nicola shared some helpful advice on how to reduce stress during a hospital stay, whether it is a scheduled stay or unexpected. While a Parkinson’s nurse aims to make sure you receive proper care, following these tips can help.
- Inform Hospital Staff: If your hospital stay is scheduled, ask if the hospital has a Parkinson’s team and inform them of your upcoming stay. In the case that they don’t have a Parkinson’s team, inform your local Parkinson’s nurse.
- Preparation: Prepare for any stay by organising yourself a ‘Get It On Time’ (GIOT) clock , and PDUK documents which may help staff on your ward understand the importance of Parkinson’s medication.
- Comfort: Bring your own clothes or pyjamas and washbag. This will ensure more comfort for yourself and encourage maintaining a good routine of getting dressed and out of bed in the morning.
- Medication List: Keep a list of your medications with you. It should detail the correct timings and dosages for your medications.
- Original Packaging: Try to bring medication that is labelled and in its original packaging. Hospitals often cannot use loose medication or medication that is in a dosette box or pill organiser. If the hospital is smaller or does not have a Parkinson’s team, they may not have your medications readily available in their pharmacy.
- Self-Administering Medicine: Ask about the hospital’s policy on self-administering medicine. If you have to take several doses per day, it may be easier to administer the medication yourself if the hospital allows it. A disruption in your medication schedule can have a big impact on how you feel, and your recovery.
- Inform Staff: Upon arrival, inform staff of your Parkinson’s diagnosis, any medication you are on, and any symptoms you are experiencing. Hospital staff are not always well versed on the details of Parkinson’s so use any tools such as the GIOT clock to help educate if possible.
- Meal Times: If you take your Parkinson’s medicine around when you eat, find out when the meal times are so that you can adjust your medication schedule.
- Medical Implants: If you have any medical implants such as deep brain stimulation (DBS), Duodopa or Apomorphine, inform staff immediately.
- Feedback: If you have a poor experience in hospital, speak to the Patient Advice and Liaison Service (PALS) or feedback team. These teams need to be aware of any areas that need improvement so that they can better this in future.
It is important to feel empowered to mention your Parkinson’s diagnosis.
No Access to a Parkinson’s Nurse?

All Parkinson’s nurses in the UK are employed by the NHS, though accessing their support differs around the UK. To find out if you have a Parkinson’s nurse available in your community, check with your GP or local doctor’s surgery. If you are seeing a clinician in the hospital, check with the hospital or your consultant. You can also check with your Parkinson’s local adviser, who may be able to refer you.
If there is no access to a Parkinson’s nurse in your area, consider the following steps to expand the support network of PD nurses:
- Parkinson’s UK Excellence Network: Parkinson’s UK runs a funding scheme for PD nurses called the Excellence Network. The process, called pump priming, sees PUK funding NHS posts. They have already supported over 325 new specialist nurse posts across the UK. Share this scheme with your clinician.
- Local Advocacy: Get your local group involved to advocate for Parkinson’s nurse support. Local groups can be found through Parkinson’s UK at this link.
- Contact Your MP: Writing to your MP can spread awareness about the support of a Parkinson’s nurse. Highlight the importance of expanding Parkinson’s care for your community.
To find out how to contact your local MP, visit this link. Parkinson’s UK also offers advice on contacting your MP and sharing your story. You can email them at: [email protected].
- Movers and Shakers Podcast: If you listen to the Movers and Shakers Podcast, you will have heard of their Parky Charter, a call on the UK government to improve the lives of people with Parkinson’s.
While ‘The Parky Charter’ has now been handed in, they welcome more signatures for those who wish to show their support. The Movers and Shakers share a lot of helpful information about Parkinson’s. You can listen to them here.
- Provide Feedback: You can provide feedback to your hospital via Patient Advice and Liaison Service (PALS). Learn more about PALS and how to contact them here.
- Contact Your ICB: Contact your local integrated care board (ICB), which is responsible for planning health services. Find your local ICB on this list.
- Parkinson’s UK Helpline: Parkinson’s UK also offers a helpline with Parkinson’s nurses. It is open Mon-Sat. Call 0808 800 0303, or visit their webpage for more information.
Thank you very much to Nicola for her talk on how to prepare for a hospital and how to take action if there are no Parkinson’s nurses in your area. To keep up to date with future Charco lectures and upcoming events, you can sign up to our newsletter here.