A landmark clinical trial, pre-published in MedRxiv, has found that Charco Neurotech’s non-invasive wearable cueing and vibrotactile stimulation device, CUE1+, delivers improvements for both motor and non-motor symptoms for people with Parkinson’s.
The trial provides robust evidence supporting real-world usability, safety/tolerability and clinical efficacy of the CUE1+ device in the management of Parkinson’s. Compared with the sham control group, participants who received the active device experienced greater and clinically meaningful improvements across motor severity, functional gait, and risk of falls, as well as non-motor symptoms, including sleep quality, self-reported impression of change, and overall quality of life. These benefits were achieved with minimal adverse effects, and positive participant experience, which are important when considering integration into routine care.
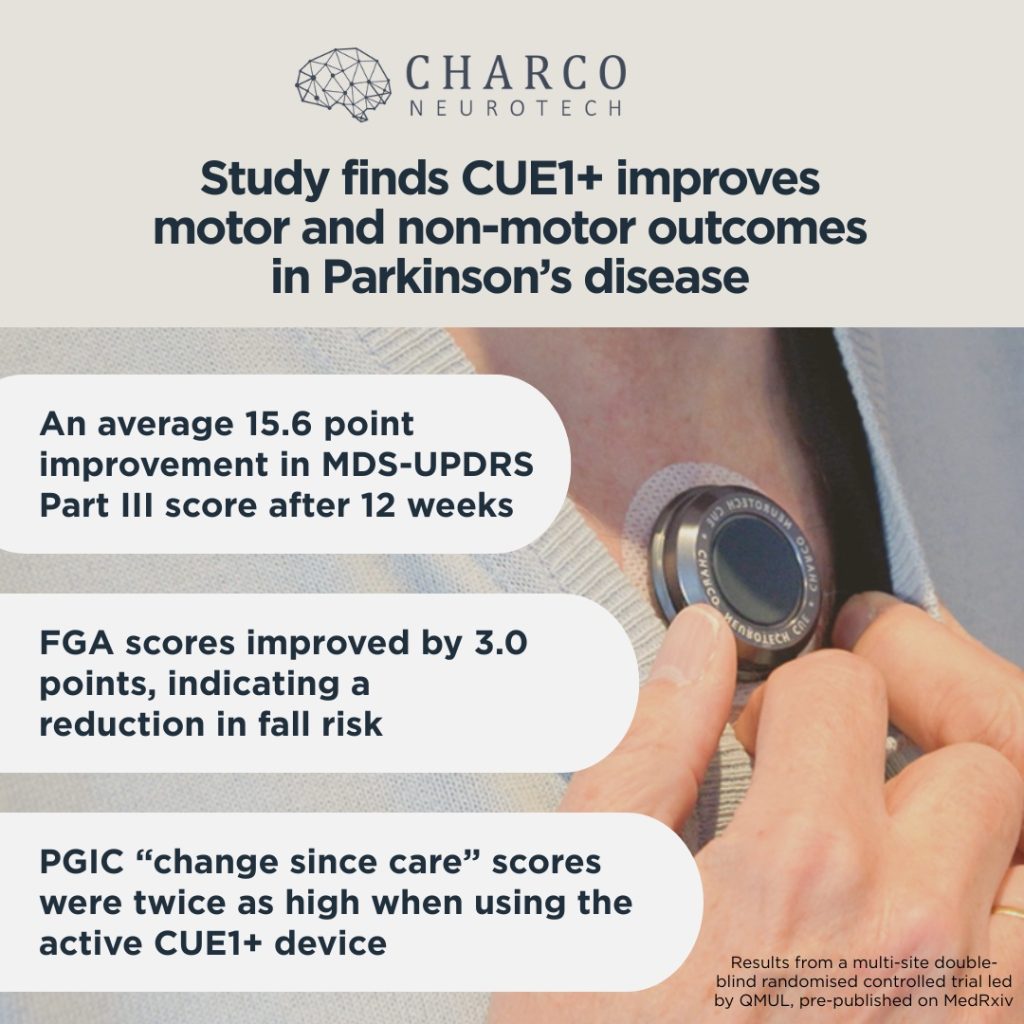
Key results include:
- Participants using the active CUE1+ device showed an average 15.6 point improvement in MDS-UPDRS Part III score (11.1 point difference from the sham group) at 12 weeks
- Functional Gait Assessment (FGA) scores improved by 3.0 points in the active group, indicating a reduction in fall risk
- Median patient global impression of care (PGIC) “change since care” score was twice as high for those in the active group
The study bodes well for Charco’s planned regulatory journey for the US, UK, and European markets. Approvals are anticipated for the first half of 2026 and this data will form part of the submission. Charco Neurotech is a UK company that develops its products in conjunction with leading neuroscientists. The company plans to expand post regulatory approval to Australia, South Korea, and the Kingdom of Saudi Arabia.
About the trial
The trial was conducted at the Centre for Preventive Neurology, Queen Mary University of London (QMUL), in collaboration with Barts Health NHS Trust and Homerton Healthcare NHS Foundation Trust.
The 12-week, double-blind, randomised controlled trial was conducted at two NHS sites in adults with idiopathic PD. Participants were randomly assigned (1:1) to receive either an active CUE1+ device or a sham device, to be worn on the sternum for 8 hours daily. Participants, investigators, and assessors were blinded to treatment allocation.
The primary outcomes were usability and safety/tolerability of CUE1+. Secondary outcomes were assessed at baseline and week 13. Motor assessments included the Movement Disorder Society-sponsored revision of the Unified Parkinson’s Disease Rating Scale (MDS-UPDRS) Part III, Functional Gait Assessment, Timed Up and Go (TUG), and two keyboard-based tapping tests, BRAIN-Kinesia Score and Digital Finger Tapping (DFT).
Patient-reported outcomes covered both motor and non-motor domains and included the MDS-UPDRS Parts I, II, and IV, Activities-specific Balance Confidence Scale (ABC), Pittsburgh Sleep Quality Index (PSQI), Parkinson’s Disease Questionnaire–39 (PDQ-39), Hospital Anxiety and Depression Scale (HADS), Fatigue Severity Scale (FSS), and Patient Global Impression of Change.
Senior authors included Cristina Simonet and Prof Alastair Noyce, with Dr Viktoria Azoidou contributing.
For access to the preprint abstract, please visit: https://www.medrxiv.org/content/10.1101/2025.07.19.25331818v1
To get in touch with the Charco Neurotech team about this study, please email [email protected]